- Diabetes, obesity and metabolism
- Glucagon-Like Peptide-1 Based Therapies: A New Horizon in Obesity Management
-
Jang Won Son, Soo Lim
-
Endocrinol Metab. 2024;39(2):206-221. Published online April 16, 2024
-
DOI: https://doi.org/10.3803/EnM.2024.1940
-
-
 Abstract Abstract
 PDF PDF PubReader PubReader  ePub ePub
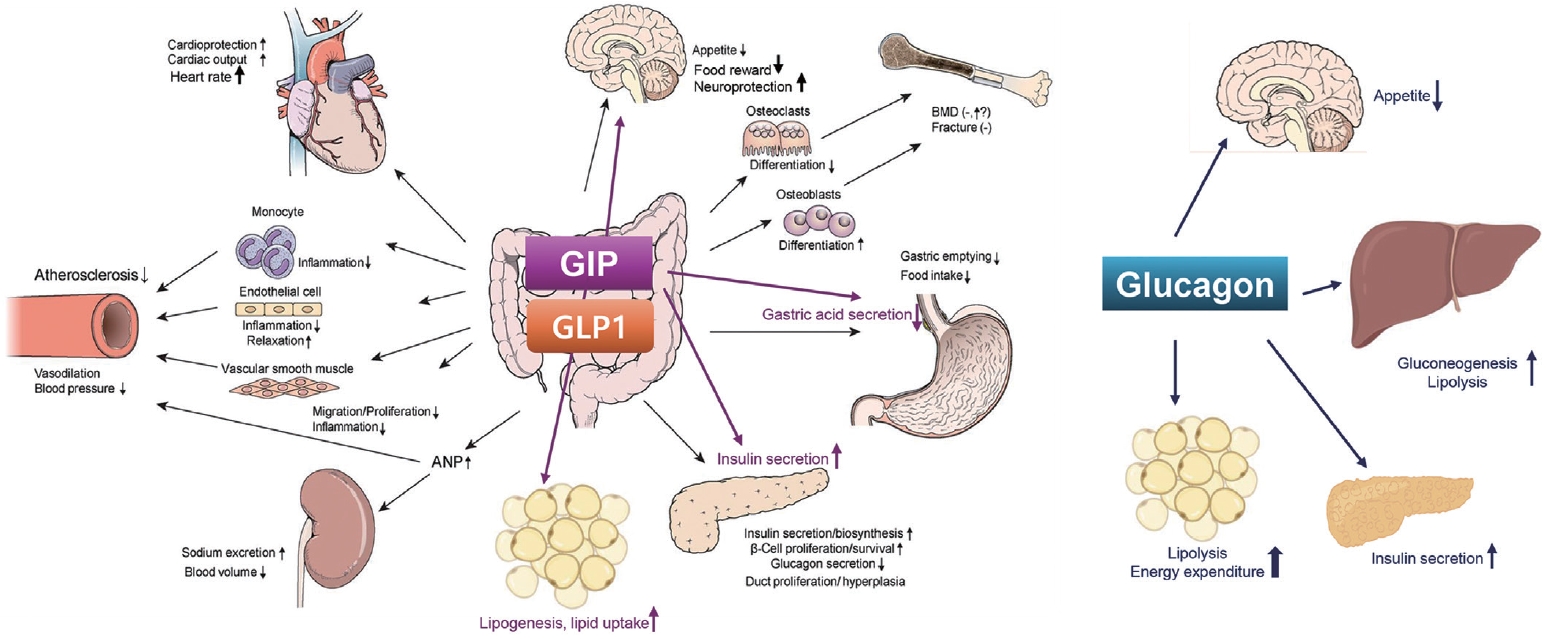
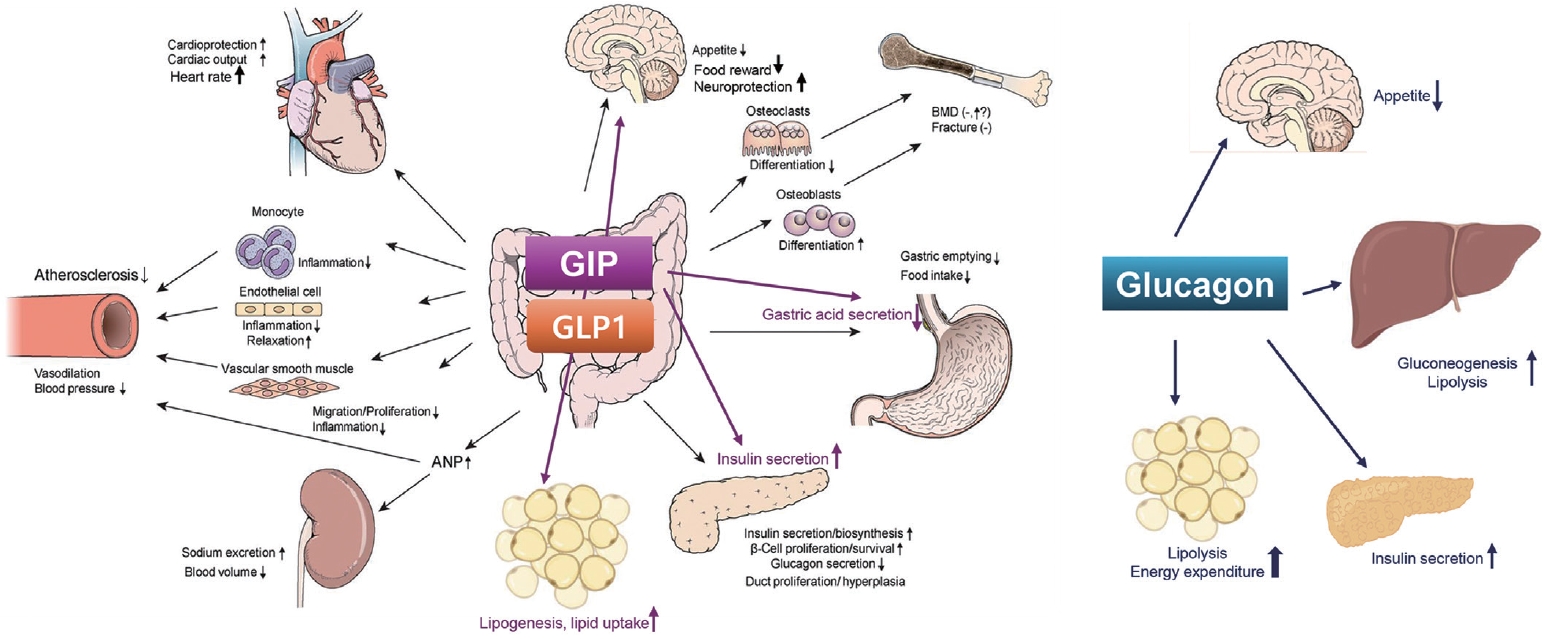
- Obesity is a significant risk factor for health issues like type 2 diabetes and cardiovascular disease. It often proves resistant to traditional lifestyle interventions, prompting a need for more precise therapeutic strategies. This has led to a focus on signaling pathways and neuroendocrine mechanisms to develop targeted obesity treatments. Recent developments in obesity management have been revolutionized by introducing novel glucagon-like peptide-1 (GLP-1) based drugs, such as semaglutide and tirzepatide. These drugs are part of an emerging class of nutrient-stimulated hormone-based therapeutics, acting as incretin mimetics to target G-protein–coupled receptors like GLP-1, glucose-dependent insulinotropic polypeptide (GIP), and glucagon. These receptors are vital in regulating body fat and energy balance. The development of multiagonists, including GLP-1–glucagon and GIP–GLP-1–glucagon receptor agonists, especially with the potential for glucagon receptor activation, marks a significant advancement in the field. This review covers the development and clinical efficacy of various GLP-1-based therapeutics, exploring the challenges and future directions in obesity management.
- Calcium & Bone Metabolism
- Comparison of Two DXA Systems, Hologic Horizon W and GE Lunar Prodigy, for Assessing Body Composition in Healthy Korean Adults
-
Seung Shin Park, Soo Lim, Hoyoun Kim, Kyoung Min Kim
-
Endocrinol Metab. 2021;36(6):1219-1231. Published online December 16, 2021
-
DOI: https://doi.org/10.3803/EnM.2021.1274
-
-
4,366
View
-
150
Download
-
3
Web of Science
-
3
Crossref
-
 Abstract Abstract
 PDF PDF Supplementary Material Supplementary Material PubReader PubReader  ePub ePub
- Background
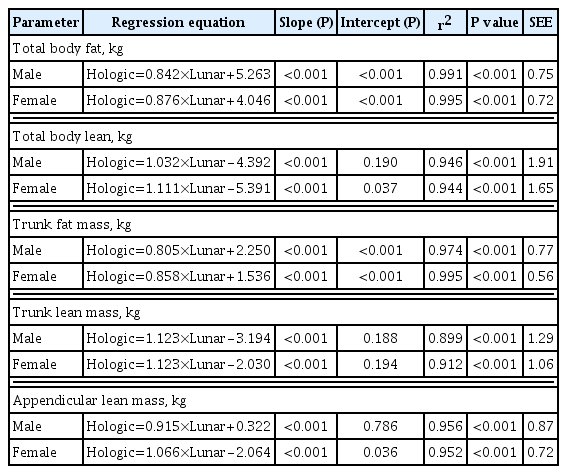
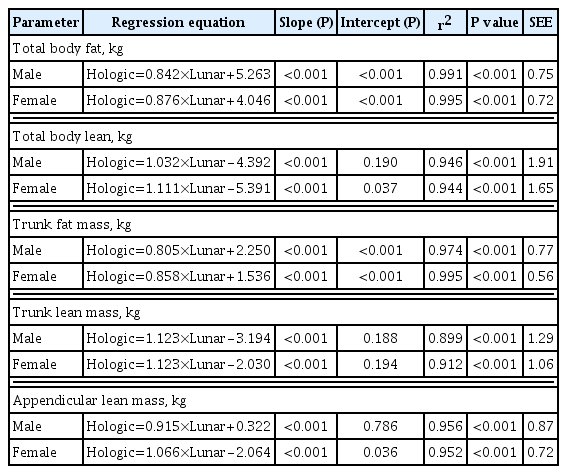
Dual-energy X-ray absorptiometry (DXA) is the most widely used method for evaluating muscle masses. The aim of this study was to investigate the agreement between muscle mass values assessed by two different DXA systems.
Methods
Forty healthy participants (20 men, 20 women; age range, 23 to 71 years) were enrolled. Total and regional body compositional values for fat and lean masses were measured consecutively with two DXA machines, Hologic Horizon and GE Lunar Prodigy. Appendicular lean mass (ALM) was calculated as the sum of the lean mass of four limbs.
Results
In both sexes, the ALM values measured by the GE Lunar Prodigy (24.8±4.3 kg in men, 15.8±2.9 kg in women) were significantly higher than those assessed by Hologic Horizon (23.0±4.0 kg in men, 14.8±3.2 kg in women). Furthermore, BMI values or body fat (%), either extremely higher or lower levels, contributed greater differences between two systems. Bland-Altman analyses revealed a significant bias between ALM values assessed by the two systems. Linear regression analyses were performed to develop equations to adjust for systematic differences (men: Horizon ALM [kg]=0.915×Lunar Prodigy ALM [kg]+0.322, R2=0.956; women: Horizon ALM [kg]=1.066×Lunar Prodigy ALM [kg]–2.064, R2=0.952).
Conclusion
Although measurements of body composition including muscle mass by the two DXA systems correlated strongly, significant differences were observed. Calibration equations should enable mutual conversion between different DXA systems.
-
Citations
Citations to this article as recorded by  - Total and regional appendicular skeletal muscle mass prediction from dual-energy X-ray absorptiometry body composition models
Cassidy McCarthy, Grant M. Tinsley, Anja Bosy-Westphal, Manfred J. Müller, John Shepherd, Dympna Gallagher, Steven B. Heymsfield
Scientific Reports.2023;[Epub] CrossRef - Cross-Calibration of iDXA and pQCT Scanners at Rural and Urban Research Sites in The Gambia, West Africa
Mícheál Ó Breasail, Ramatoulie Janha, Ayse Zengin, Camille Pearse, Landing Jarjou, Ann Prentice, Kate A. Ward
Calcified Tissue International.2023; 112(5): 573. CrossRef - Estimation of Absolute and Relative Body Fat Content Using Noninvasive Surrogates: Can DXA Be Bypassed?
David J. Greenblatt, Christopher D. Bruno, Jerold S. Harmatz, Bess Dawson‐Hughes, Qingchen Zhang, Chunhui Li, Christina R. Chow
The Journal of Clinical Pharmacology.2023;[Epub] CrossRef
- Endocrine Research
- Effects of Glucagon-Like Peptide-1 Analogue and Fibroblast Growth Factor 21 Combination on the Atherosclerosis-Related Process in a Type 2 Diabetes Mouse Model
-
Jin Hee Kim, Gha Young Lee, Hyo Jin Maeng, Hoyoun Kim, Jae Hyun Bae, Kyoung Min Kim, Soo Lim
-
Endocrinol Metab. 2021;36(1):157-170. Published online February 24, 2021
-
DOI: https://doi.org/10.3803/EnM.2020.781
-
-
6,871
View
-
176
Download
-
10
Web of Science
-
11
Crossref
-
 Abstract Abstract
 PDF PDF Supplementary Material Supplementary Material PubReader PubReader  ePub ePub
- Background
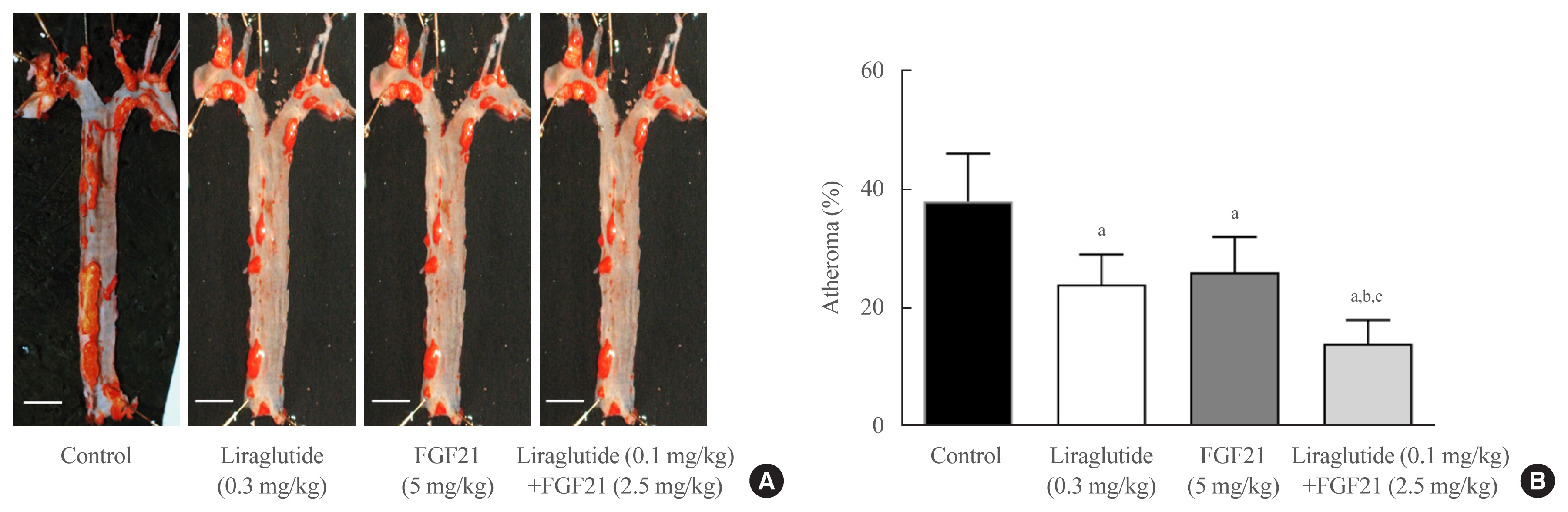
Glucagon-like peptide-1 (GLP-1) analogues regulate glucose homeostasis and have anti-inflammatory properties, but cause gastrointestinal side effects. The fibroblast growth factor 21 (FGF21) is a hormonal regulator of lipid and glucose metabolism that has poor pharmacokinetic properties, including a short half-life. To overcome these limitations, we investigated the effect of a low-dose combination of a GLP-1 analogue and FGF21 on atherosclerosis-related molecular pathways.
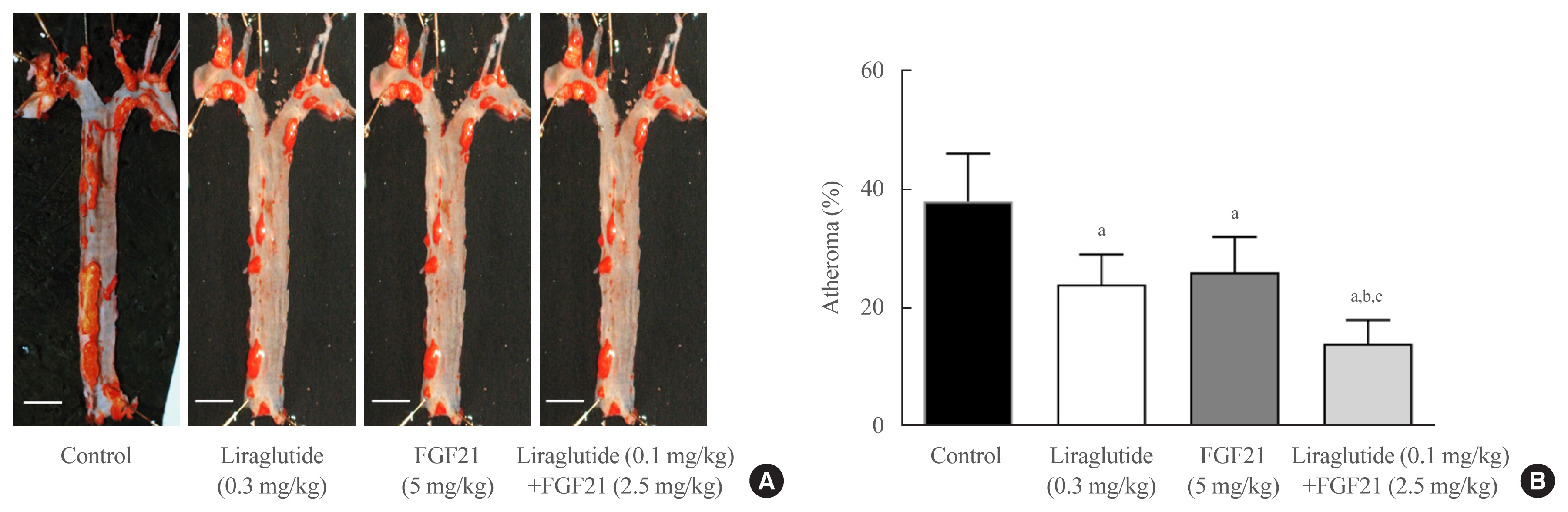
Methods
C57BL/6J mice were fed a high-fat diet for 30 weeks followed by an atherogenic diet for 10 weeks and were divided into four groups: control (saline), liraglutide (0.3 mg/kg/day), FGF21 (5 mg/kg/day), and low-dose combination treatment with liraglutide (0.1 mg/kg/day) and FGF21 (2.5 mg/kg/day) (n=6/group) for 6 weeks. The effects of each treatment on various atherogenesisrelated pathways were assessed.
Results
Liraglutide, FGF21, and their low-dose combination significantly reduced atheromatous plaque in aorta, decreased weight, glucose, and leptin levels, and increased adiponectin levels. The combination treatment upregulated the hepatic uncoupling protein-1 (UCP1) and Akt1 mRNAs compared with controls. Matric mentalloproteinase-9 (MMP-9), monocyte chemoattractant protein-1 (MCP-1), and intercellular adhesion molecule-1 (ICAM-1) were downregulated and phosphorylated Akt (p-Akt) and phosphorylated extracellular signal-regulated kinase (p-ERK) were upregulated in liver of the liraglutide-alone and combination-treatment groups. The combination therapy also significantly decreased the proliferation of vascular smooth muscle cells. Caspase-3 was increased, whereas MMP-9, ICAM-1, p-Akt, and p-ERK1/2 were downregulated in the liraglutide-alone and combination-treatment groups.
Conclusion
Administration of a low-dose GLP-1 analogue and FGF21 combination exerts beneficial effects on critical pathways related to atherosclerosis, suggesting the synergism of the two compounds.
-
Citations
Citations to this article as recorded by  - Current status and future perspectives of FGF21 analogues in clinical trials
Zara Siu Wa Chui, Qing Shen, Aimin Xu
Trends in Endocrinology & Metabolism.2024;[Epub] CrossRef - Design and pharmaceutical evaluation of bifunctional fusion protein of FGF21 and GLP-1 in the treatment of nonalcoholic steatohepatitis
Xianlong Ye, Yingli Chen, Jianying Qi, Shenglong Zhu, Yuanyuan Wu, Jingjing Xiong, Fei Hu, Zhimou Guo, Xinmiao Liang
European Journal of Pharmacology.2023; 952: 175811. CrossRef - Use of FGF21 analogs for the treatment of metabolic disorders: a systematic review and meta-analysis
Maria Paula Carbonetti, Fernanda Almeida-Oliveira, David Majerowicz
Archives of Endocrinology and Metabolism.2023;[Epub] CrossRef - Exploring the potential mechanism of Simiao Yongan decoction in the treatment of diabetic peripheral vascular disease based on network pharmacology and molecular docking technology
Fang Cao, Yongkang Zhang, Yuan Zong, Xia Feng, Junlin Deng, Yuzhen Wang, Yemin Cao
Medicine.2023; 102(52): e36762. CrossRef - The Healing Capability of Clove Flower Extract (CFE) in Streptozotocin-Induced (STZ-Induced) Diabetic Rat Wounds Infected with Multidrug Resistant Bacteria
Rewaa Ali, Tarek Khamis, Gamal Enan, Gamal El-Didamony, Basel Sitohy, Gamal Abdel-Fattah
Molecules.2022; 27(7): 2270. CrossRef - Nonalcoholic Steatohepatitis (NASH) and Atherosclerosis: Explaining Their Pathophysiology, Association and the Role of Incretin-Based Drugs
Eleftheria Galatou, Elena Mourelatou, Sophia Hatziantoniou, Ioannis S. Vizirianakis
Antioxidants.2022; 11(6): 1060. CrossRef - Unlocking the Therapeutic Potential of Glucagon-Like Peptide-1 Analogue and Fibroblast Growth Factor 21 Combination for the Pathogenesis of Atherosclerosis in Type 2 Diabetes
Jang Won Son
Endocrinology and Metabolism.2021; 36(1): 57. CrossRef - Effects of fasting on skeletal muscles and body fat of adult and old C57BL/6J mice
Mindaugas Kvedaras, Petras Minderis, Leonardo Cesanelli, Agne Cekanauskaite, Aivaras Ratkevicius
Experimental Gerontology.2021; 152: 111474. CrossRef - The Role of Fibroblast Growth Factor 21 in Diabetic Cardiovascular Complications and Related Epigenetic Mechanisms
Mengjie Xiao, Yufeng Tang, Shudong Wang, Jie Wang, Jie Wang, Yuanfang Guo, Jingjing Zhang, Junlian Gu
Frontiers in Endocrinology.2021;[Epub] CrossRef - Liraglutide Decreases Liver Fat Content and Serum Fibroblast Growth Factor 21 Levels in Newly Diagnosed Overweight Patients with Type 2 Diabetes and Nonalcoholic Fatty Liver Disease
Xinyue Li, Xiaojuan Wu, Yumei Jia, Jing Fu, Lin Zhang, Tao Jiang, Jia Liu, Guang Wang, Claudia Cardoso
Journal of Diabetes Research.2021; 2021: 1. CrossRef - Differential importance of endothelial and hematopoietic cell GLP-1Rs for cardiometabolic versus hepatic actions of semaglutide
Brent A. McLean, Chi Kin Wong, Kiran Deep Kaur, Randy J. Seeley, Daniel J. Drucker
JCI Insight.2021;[Epub] CrossRef
- Clinical Study
- Glycemic Efficacy and Metabolic Consequences of an Empagliflozin Add-on versus Conventional Dose-Increasing Strategy in Patients with Type 2 Diabetes Inadequately Controlled by Metformin and Sulfonylurea
-
Yujin Shin, Ji Hye Moon, Ho Jun Chin, Ele Ferrannini, Soo Lim
-
Endocrinol Metab. 2020;35(2):329-338. Published online June 24, 2020
-
DOI: https://doi.org/10.3803/EnM.2020.35.2.329
-
-
6,551
View
-
215
Download
-
10
Web of Science
-
7
Crossref
-
 Abstract Abstract
 PDF PDF Supplementary Material Supplementary Material PubReader PubReader  ePub ePub
- Background
We assessed the glucose-lowering efficacy of adding empagliflozin versus dose escalating existing medications in patients with uncontrolled type 2 diabetes (T2D).
Methods
This was a 6-month retrospective case-control study in subjects with uncontrolled T2D (glycated hemoglobin [HbA1c] >7%) on conventional treatment. The study group started add-on therapy with empagliflozin (10 mg once a day) while the control group was up-titrated with existing medication, using either monotherapy or a combination of metformin, sulfonylurea, and a dipeptidyl peptidase-4 inhibitor. The primary endpoints included changes in HbA1c, fasting plasma glucose (FPG), and 2-hour postprandial glucose (PP2) levels. Secondary outcomes included changes in body composition, body mass index (BMI), and serum ketone bodies, and urinary excretion of sodium, potassium, chlorine, calcium, phosphorus, and glucose.
Results
After treatment, the reduction in HbA1c was significantly greater in the empagliflozin group than in controls (from 8.6%±1.6% to 7.6%±1.5% vs. 8.5%±1.1% to 8.1%±1.1%; P<0.01). Similar patterns were found in FPG and PP2 levels. Empagliflozin decreased systolic and diastolic blood pressure, triglycerides, and alanine and aspartate aminotransferase levels. Body weight, BMI, waist circumference, fat mass, and abdominal visceral fat area decreased significantly while lean body mass was maintained. Total ketones, β-hydroxybutyrate, and acetoacetate levels increased significantly after empagliflozin.
Conclusion
In addition to glucose lowering, an empagliflozin add-on regimen decreased blood pressure and body fat, and improved metabolic profiles significantly. Empagliflozin add-on is superior to dose escalation in patients with T2D who have inadequate glycemic control on standard medications.
-
Citations
Citations to this article as recorded by  - Independent association of thigh muscle fat density with vascular events in Korean adults
Hun Jee Choe, Won Chang, Matthias Blüher, Steven B. Heymsfield, Soo Lim
Cardiovascular Diabetology.2024;[Epub] CrossRef - Sodium glucose co-transporter-2 inhibitor, Empagliflozin, is associated with significant reduction in weight, body mass index, fasting glucose, and A1c levels in Type 2 diabetic patients with established coronary heart disease: the SUPER GATE study
Satilmis Bilgin, Ozge Kurtkulagi, Tuba Taslamacioglu Duman, Burcin Meryem Atak Tel, Gizem Kahveci, Murat Kiran, Eray Erge, Gulali Aktas
Irish Journal of Medical Science (1971 -).2022; 191(4): 1647. CrossRef - A randomized clinical trial evaluating the effect of empagliflozin on triglycerides in obese adults: Role of visceral fat
Min Hee Lee, Ian J. Neeland, Natalia de Albuquerque Rocha, Connor Hughes, Craig R. Malloy, Eunsook S. Jin
Metabolism Open.2022; 13: 100161. CrossRef - Initial combination of metformin, sitagliptin, and empagliflozin in drug‐naïve patients with type 2 diabetes: Safety and metabolic effects
Soo Lim, Minji Sohn, Yujin Shin, Ele Ferrannini
Diabetes, Obesity and Metabolism.2022; 24(4): 757. CrossRef - Correlation of dynamic membrane fluctuations in red blood cells with diabetes mellitus and cardiovascular risks
Minji Sohn, Ji Eun Lee, MinGeun Ahn, YongKeun Park, Soo Lim
Scientific Reports.2021;[Epub] CrossRef - Comparison betweeen dapagliflozin add-on therapy and insulin dose escalation in patients with uncontrolled type 2 diabetes treated with insulin: DVI study
Yujin Shin, Haeri Choi, Soo Lim
Diabetes Research and Clinical Practice.2021; 175: 108843. CrossRef - Impact of COVID-19 and Associated Preventive Measures on Cardiometabolic Risk Factors in South Korea
Minji Sohn, Bo Kyung Koo, Ho Il Yoon, Kyoung-Ho Song, Eu Suk Kim, Hong Bin Kim, Soo Lim
Journal of Obesity & Metabolic Syndrome.2021; 30(3): 248. CrossRef
- Clinical Study
- Effect of Lactobacillus sakei, a Probiotic Derived from Kimchi, on Body Fat in Koreans with Obesity: A Randomized Controlled Study
-
Soo Lim, Ji Hye Moon, Chol Min Shin, Dahye Jeong, Bongjoon Kim
-
Endocrinol Metab. 2020;35(2):425-434. Published online June 24, 2020
-
DOI: https://doi.org/10.3803/EnM.2020.35.2.425
-
-
8,651
View
-
261
Download
-
30
Web of Science
-
34
Crossref
-
 Abstract Abstract
 PDF PDF PubReader PubReader  ePub ePub
- Background
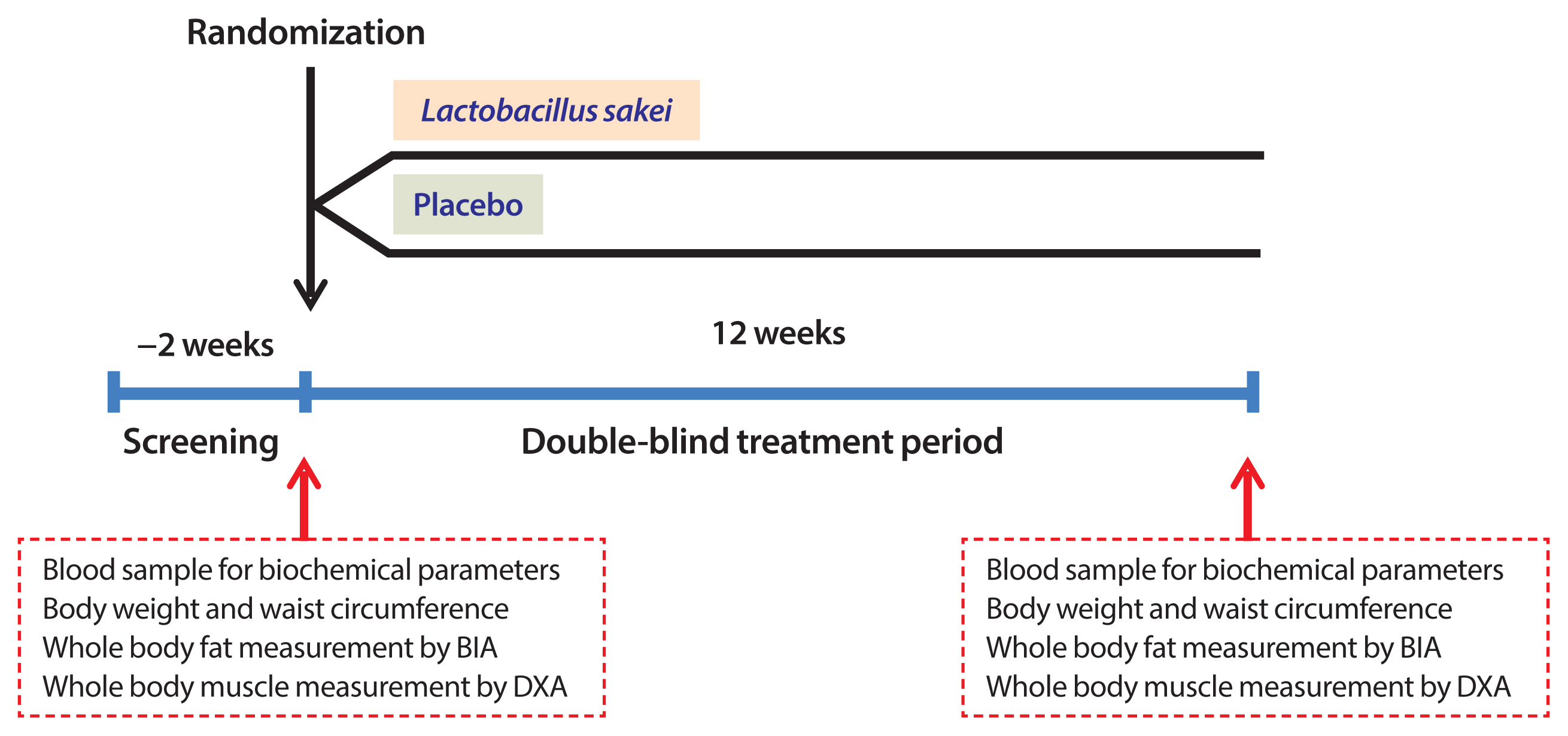
The increased prevalence of obesity has led to increases in the prevalence of chronic diseases worldwide. There is interest whether probiotics have an effect on obesity, but the effectiveness and safety of only a few probiotics for the treatment of obesity have been reported. The purpose of this study was to investigate whether ingestion of Lactobacillus sakei (CJLS03) derived from kimchi causes weight loss in people with obesity.
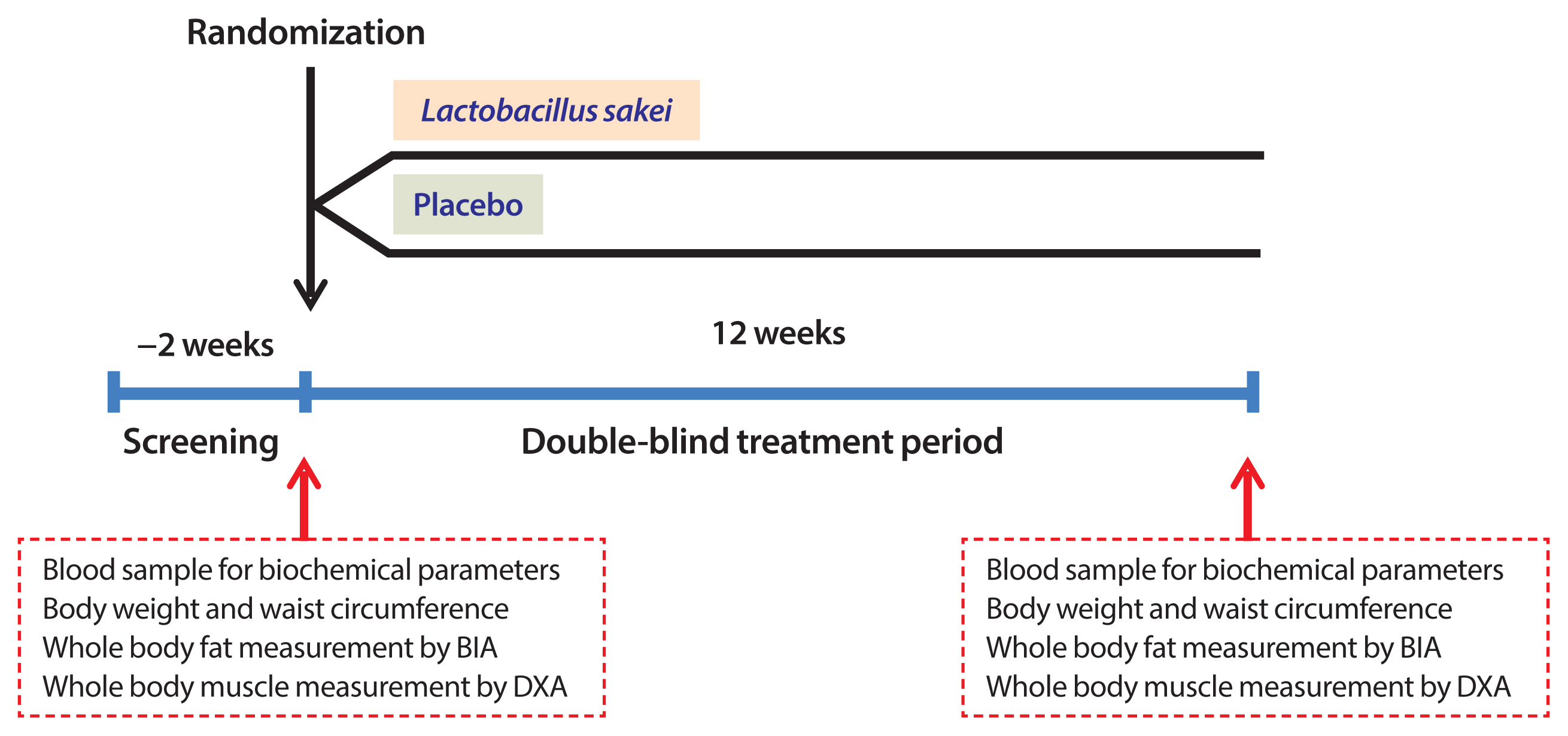
Methods
This randomized, double-blind, placebo-controlled, clinical trial involved 114 adults with a body mass index (BMI) ≥25 kg/m2 who were assigned randomly to a CJLS03 or placebo group. The groups received two allocations of either 5×109 colony-forming units of CJLS03/allocation or the equivalent vehicle for 12 weeks. Demographic and biochemical parameters, and body composition including fat and muscle mass were measured at baseline and after 12 weeks. Changes in body fat, weight, and waist circumference were compared between the two treatment groups. Adverse events were monitored during study period.
Results
Body fat mass decreased by 0.2 kg in the CJLS03 group and increased by 0.6 kg in the placebo group (0.8 kg difference, P=0.018). After the 12 weeks, waist circumference was 0.8 cm smaller in the CJLS03 group than in the placebo group (P=0.013). BMI and body weight did not change after the 12 weeks. Adverse events were mild and did not differ between the two groups.
Conclusion
These data suggest that L. sakei (CJLS03) might help people with obesity reduce body fat mass without serious side effects (ClinicalTrials.gov: NCT03248414).
-
Citations
Citations to this article as recorded by  -
Latilactobacillus sakei
: a candidate probiotic with a key role in food fermentations and health promotion
Leilei Yu, Ying Chen, Hui Duan, Nanzhen Qiao, Gang Wang, Jianxin Zhao, Qixiao Zhai, Fengwei Tian, Wei Chen
Critical Reviews in Food Science and Nutrition.2024; 64(4): 978. CrossRef - Beneficial effects of the probiotics and synbiotics supplementation on anthropometric indices and body composition in adults: A systematic review and meta‐analysis
Saeede Saadati, Kaveh Naseri, Omid Asbaghi, Mohsen Yousefi, Elnaz Golalipour, Barbora de Courten
Obesity Reviews.2024;[Epub] CrossRef - Spore-forming probiotics Weizmannia coagulans isolated from human breast milk improves on the flavor development using micro-cheese platform
Hyejin Choi, Daye Mun, Sangdon Ryu, Min-Jin Kwak, Bum-Keun Kim, Dong-Jun Park, Do-Youn Jeong, Wonseo Park, Sangnam Oh, Younghoon Kim
Food Bioscience.2024; 57: 103550. CrossRef - Latilactobacillus sakei as a starter culture to ferment pepper fruits
Emma Mani-López, Nelly Ramírez-Corona, Aurelio López-Malo
Food and Humanity.2024; 2: 100233. CrossRef - Association between kimchi consumption and obesity based on BMI and abdominal obesity in Korean adults: a cross-sectional analysis of the Health Examinees study
Hyein Jung, Ye-Rang Yun, Sung Wook Hong, Sangah Shin
BMJ Open.2024; 14(2): e076650. CrossRef - Adjunctive administration of parabiotic Lactobacillus sakei CVL-001 ameliorates drug-induced toxicity and pulmonary inflammation during antibiotic treatment for tuberculosis
Hagyu Kim, Eun-Jung Song, Eunsol Choi, Kee Woong Kwon, Jong-Hwan Park, Sung Jae Shin
International Immunopharmacology.2024; 132: 111937. CrossRef - Anti-obesogenic effects of plant natural products: A focus on Korean traditional foods
Gitishree Das, Luis Alfonso Jiménez Ortega, Sandra Gonçalves, J. Basilio Heredia, Maria de Lourdes Gomes Pereira, Anabela Romano, Han-Seung Shin, Jayanta Kumar Patra
Trends in Food Science & Technology.2024; : 104470. CrossRef - The effect of probiotic and synbiotic supplementation on lipid parameters among patients with cardiometabolic risk factors: a systematic review and meta-analysis of clinical trials
Zeinab Ghorbani, Asma Kazemi, Theda U.P. Bartolomaeus, Fahimeh Martami, Morvarid Noormohammadi, Arsalan Salari, Ulrike Löber, Heydar Ali Balou, Sofia K. Forslund, Marjan Mahdavi-Roshan
Cardiovascular Research.2023; 119(4): 933. CrossRef - Impact of probiotics on muscle mass, muscle strength and lean mass: a systematic review and meta‐analysis of randomized controlled trials
Konstantinos Prokopidis, Panagiotis Giannos, Richard Kirwan, Theocharis Ispoglou, Francesco Galli, Oliver C. Witard, Konstantinos K. Triantafyllidis, Konstantinos S. Kechagias, Jordi Morwani‐Mangnani, Andrea Ticinesi, Masoud Isanejad
Journal of Cachexia, Sarcopenia and Muscle.2023; 14(1): 30. CrossRef - Anti-obesity potential of heat-killed Lactiplantibacillus plantarum K8 in 3T3-L1 cells and high-fat diet mice
Kyoung Ok Jang, Jung Seo Choi, Kyeong Hun Choi, Seongjae Kim, Hangeun Kim, Dae Kyun Chung
Heliyon.2023; 9(1): e12926. CrossRef - Effect of Lactobacillus plantarum LMT1-48 on Body Fat in Overweight Subjects: A Randomized, Double-Blind, Placebo-Controlled Trial
Minji Sohn, Hyeyoung Jung, Woo Shun Lee, Tai Hoon Kim, Soo Lim
Diabetes & Metabolism Journal.2023; 47(1): 92. CrossRef - Effect of kimchi intake on body weight of general community dwellers: a prospective cohort study
Li-Juan Tan, Ye-Rang Yun, Sung Wook Hong, Sangah Shin
Food & Function.2023; 14(4): 2162. CrossRef - Effects of Probiotics on Intermediate Cardiovascular Outcomes in Patients with Overweight or Obesity: A Systematic Review and Meta-Analysis
Frank Mayta-Tovalino, Carlos Diaz-Arocutipa, Alejandro Piscoya, Adrian V. Hernandez
Journal of Clinical Medicine.2023; 12(7): 2554. CrossRef - Effects of kimchi on human health: a scoping review of randomized controlled trials
Eunhye Song, Lin Ang, Hye Won Lee, Myung-Sunny Kim, You Jin Kim, Daija Jang, Myeong Soo Lee
Journal of Ethnic Foods.2023;[Epub] CrossRef - Randomized controlled trials reporting the effects of probiotics in individuals with overweight and obesity: A critical review of the interventions and body adiposity parameters
Marcella Rodrigues Guedes, Karine Scanci da Silva Pontes, Maria Inês Barreto Silva, Mario Fritsch Neves, Márcia Regina Simas Torres Klein
Clinical Nutrition.2023; 42(6): 835. CrossRef - Roles of the gut microbiome in weight management
Rachel N. Carmody, Jordan E. Bisanz
Nature Reviews Microbiology.2023; 21(8): 535. CrossRef - Does gut microbiota affect the success of weight loss? Evidence and speculation
Małgorzata Moszak, Marta Pelczyńska, Agnieszka Wesołek, Dominika Stenclik, Paweł Bogdański
Nutrition.2023; 116: 112111. CrossRef - Certain Fermented Foods and Their Possible Health Effects with a Focus on Bioactive Compounds and Microorganisms
Gülsüm Deveci, Elif Çelik, Duygu Ağagündüz, Elena Bartkiene, João Miguel F. Rocha, Fatih Özogul
Fermentation.2023; 9(11): 923. CrossRef - The gut microbiome in the fight against obesity: The potential of dietary factors
Jamil Ahmad, Imran Khan, Gokhan Zengin, Mohamad Fawzi Mahomoodally
The FASEB Journal.2023;[Epub] CrossRef - Effect of Continuous Ingestion of Bifidobacteria and Inulin on Reducing Body Fat: A Randomized, Double-Blind, Placebo-Controlled, Parallel-Group Comparison Study
Yuhei Baba, Yasuo Saito, Mei Kadowaki, Naoki Azuma, Daisuke Tsuge
Nutrients.2023; 15(24): 5025. CrossRef - A Review of the Health Benefits of Kimchi Functional Compounds and Metabolites
Hyun Ju Kim, Min Sung Kwon, Hyelyeon Hwang, Ha-Sun Choi, WooJe Lee, Sang-Pil Choi, Haeun Jo, Sung Wook Hong
Microbiology and Biotechnology Letters.2023; 51(4): 353. CrossRef - Efficacy and Safety of Lactobacillus plantarum K50 on Lipids in Koreans With Obesity: A Randomized, Double-Blind Controlled Clinical Trial
Minji Sohn, Ga Yoon Na, Jaeryang Chu, Hyunchae Joung, Byung-Kook Kim, Soo Lim
Frontiers in Endocrinology.2022;[Epub] CrossRef - Changes in systolic blood pressure, postprandial glucose, and gut microbial composition following mango consumption in individuals with overweight and obesity
Justine Keathley, Michèle Kearney, Véronique Garneau, Juan de Toro-Martín, Thibault V. Varin, Geneviève Pilon, Patrick Couture, André Marette, Marie-Claude Vohl, Charles Couillard
Applied Physiology, Nutrition, and Metabolism.2022; 47(5): 565. CrossRef - Host—microbial interactions in metabolic diseases: from diet to immunity
Ju-Hyung Lee, Joo-Hong Park
Journal of Microbiology.2022; 60(6): 561. CrossRef - Effect of MED-02 Containing Two Probiotic Strains, Limosilactobacillus fermentum MG4231 and MG4244, on Body Fat Reduction in Overweight or Obese Subjects: A Randomized, Multicenter, Double-Blind, Placebo-Controlled Study
Young Gyu Cho, Yun Jun Yang, Yeong Sook Yoon, Eon Sook Lee, Jun Hyung Lee, Yulah Jeong, Chang Ho Kang
Nutrients.2022; 14(17): 3583. CrossRef - Evaluation of metabolic activities and probiotic characteristics of two Latilactobacillus sakei strains isolated from pastırma
Emine Dincer, Merih Kivanc
World Journal of Microbiology and Biotechnology.2022;[Epub] CrossRef - Correlation between autochthonous microbial communities and flavor profiles during the fermentation of mustard green paocai (Brassica juncea Coss.), a typical industrial-scaled salted fermented vegetable
Dongdong Wang, Gong Chen, Yao Tang, Jiayi Li, Runqiu Huang, Meizuo Ye, Jianying Ming, Yalong Wu, Fei Xu, Xingyue Lai, Qisheng Zhang, Wenxue Zhang
LWT.2022; 172: 114212. CrossRef - Therapeutic and Improving Function of Lactobacilli in the Prevention and Treatment of Cardiovascular-Related Diseases: A Novel Perspective From Gut Microbiota
Xin Zhao, Xinqin Zhong, Xiao Liu, Xiaoying Wang, Xiumei Gao
Frontiers in Nutrition.2021;[Epub] CrossRef - Don’t Worry, Heavy Moms; Just Eat Your Broccoli (or Kimchi)!
Sun-Kyung Lee
Molecules and Cells.2021; 44(6): 422. CrossRef - Effects of probiotics on body adiposity and cardiovascular risk markers in individuals with overweight and obesity: A systematic review and meta-analysis of randomized controlled trials
Karine Scanci da Silva Pontes, Marcella Rodrigues Guedes, Michelle Rabello da Cunha, Samanta de Souza Mattos, Maria Inês Barreto Silva, Mario Fritsch Neves, Bianca Cristina Antunes Alves Marques, Márcia Regina Simas Torres Klein
Clinical Nutrition.2021; 40(8): 4915. CrossRef - Health-Promoting Constituents and Selected Quality Parameters of Different Types of Kimchi: Fermented Plant Products
Anna Korus, Emilia Bernaś, Jarosław Korus, Eduard Hernández
International Journal of Food Science.2021; 2021: 1. CrossRef - Effects of Probiotics and Synbiotics on Weight Loss in Subjects with Overweight or Obesity: A Systematic Review
Valentina Álvarez-Arraño, Sandra Martín-Peláez
Nutrients.2021; 13(10): 3627. CrossRef - ADJUVANT AND BENEFICIAL PROBIOTIC THERAPY FOR WOMEN HEALTH
Igori Balta, Eugenia Butucel, Valentyn Mohylyuk
Romanian Archives of Microbiology and Immunology.2021; 80(2): 151. CrossRef - Nrf2-interacting nutrients and COVID-19: time for research to develop adaptation strategies
Jean Bousquet, Jean-Paul Cristol, Wienczyslawa Czarlewski, Josep M. Anto, Adrian Martineau, Tari Haahtela, Susana C. Fonseca, Guido Iaccarino, Hubert Blain, Alessandro Fiocchi, G. Walter Canonica, Joao A. Fonseca, Alain Vidal, Hak-Jong Choi, Hyun Ju Kim,
Clinical and Translational Allergy.2020;[Epub] CrossRef
- Thyroid
- Validity and Reliability of the Korean Version of the Hyperthyroidism Symptom Scale
-
Jie-Eun Lee, Dong Hwa Lee, Tae Jung Oh, Kyoung Min Kim, Sung Hee Choi, Soo Lim, Young Joo Park, Do Joon Park, Hak Chul Jang, Jae Hoon Moon
-
Endocrinol Metab. 2018;33(1):70-78. Published online March 21, 2018
-
DOI: https://doi.org/10.3803/EnM.2018.33.1.70
-
-
4,057
View
-
55
Download
-
3
Web of Science
-
3
Crossref
-
 Abstract Abstract
 PDF PDF PubReader PubReader  ePub ePub
- Background
Thyrotoxicosis is a common disease resulting from an excess of thyroid hormones, which affects many organ systems. The clinical symptoms and signs are relatively nonspecific and can vary depending on age, sex, comorbidities, and the duration and cause of the disease. Several symptom rating scales have been developed in an attempt to assess these symptoms objectively and have been applied to diagnosis or to evaluation of the response to treatment. The aim of this study was to assess the reliability and validity of the Korean version of the hyperthyroidism symptom scale (K-HSS). MethodsTwenty-eight thyrotoxic patients and 10 healthy subjects completed the K-HSS at baseline and after follow-up at Seoul National University Bundang Hospital. The correlation between K-HSS scores and thyroid function was analyzed. K-HSS scores were compared between baseline and follow-up in patient and control groups. Cronbach's α coefficient was calculated to demonstrate the internal consistency of K-HSS. ResultsThe mean age of the participants was 34.7±9.8 years and 13 (34.2%) were men. K-HSS scores demonstrated a significant positive correlation with serum free thyroxine concentration and decreased significantly with improved thyroid function. K-HSS scores were highest in subclinically thyrotoxic subjects, lower in patients who were euthyroid after treatment, and lowest in the control group at follow-up, but these differences were not significant. Cronbach's α coefficient for the K-HSS was 0.86. ConclusionThe K-HSS is a reliable and valid instrument for evaluating symptoms of thyrotoxicosis in Korean patients.
-
Citations
Citations to this article as recorded by  - Effect of thyroid-stimulating hormone suppression on quality of life in thyroid lobectomy patients: interim analysis of a multicenter, randomized controlled trial in low- to intermediate-risk thyroid cancer patients (MASTER study)
Ja Kyung Lee, Eu Jeong Ku, Su-jin Kim, Woochul Kim, Jae Won Cho, Kyong Yeun Jung, Hyeong Won Yu, Yea Eun Kang, Mijin Kim, Hee Kyung Kim, Junsun Ryu, June Young Choi
Annals of Surgical Treatment and Research.2024; 106(1): 19. CrossRef - Effect of increased levothyroxine dose on depressive mood in older adults undergoing thyroid hormone replacement therapy
Jae Hoon Moon, Ji Won Han, Tae Jung Oh, Sung Hee Choi, Soo Lim, Ki Woong Kim, Hak Chul Jang
Clinical Endocrinology.2020; 93(2): 196. CrossRef - Clinical Feasibility of Monitoring Resting Heart Rate Using a Wearable Activity Tracker in Patients With Thyrotoxicosis: Prospective Longitudinal Observational Study
Jie-Eun Lee, Dong Hwa Lee, Tae Jung Oh, Kyoung Min Kim, Sung Hee Choi, Soo Lim, Young Joo Park, Do Joon Park, Hak Chul Jang, Jae Hoon Moon
JMIR mHealth and uHealth.2018; 6(7): e159. CrossRef
- Endocrine Research
- Effects of Lobeglitazone, a New Thiazolidinedione, on Osteoblastogenesis and Bone Mineral Density in Mice
-
Kyoung Min Kim, Hyun-Jin Jin, Seo Yeon Lee, Hyo Jin Maeng, Gha Young Lee, Tae Jung Oh, Sung Hee Choi, Hak Chul Jang, Soo Lim
-
Endocrinol Metab. 2017;32(3):389-395. Published online September 18, 2017
-
DOI: https://doi.org/10.3803/EnM.2017.32.3.389
-
-
4,781
View
-
51
Download
-
11
Web of Science
-
10
Crossref
-
 Abstract Abstract
 PDF PDF PubReader PubReader
- Background
Bone strength is impaired in patients with type 2 diabetes mellitus despite an increase in bone mineral density (BMD). Thiazolidinedione (TZD), a peroxisome proliferator activated receptor γ agonist, promotes adipogenesis, and suppresses osteoblastogenesis. Therefore, its use is associated with an increased risk of fracture. The aim of this study was to examine the in vitro and in vivo effects of lobeglitazone, a new TZD, on bone. MethodsMC3T3E1 and C3H10T1/2 cells were cultured in osteogenic medium and exposed to lobeglitazone (0.1 or 1 µM), rosiglitazone (0.4 µM), or pioglitazone (1 µM) for 10 to 14 days. Alkaline phosphatase (ALP) activity, Alizarin red staining, and osteoblast marker gene expression were analyzed. For in vivo experiments, 6-month-old C57BL/6 mice were treated with vehicle, one of two doses of lobeglitazone, rosiglitazone, or pioglitazone. BMD was assessed using a PIXImus2 instrument at the baseline and after 12 weeks of treatment. ResultsAs expected, in vitro experiments showed that ALP activity was suppressed and the mRNA expression of osteoblast marker genes RUNX2 (runt-related transcription factor 2) and osteocalcin was significantly attenuated after rosiglitazone treatment. By contrast, lobeglitazone at either dose did not inhibit these variables. Rosiglitazone-treated mice showed significantly accelerated bone loss for the whole bone and femur, but BMD did not differ significantly between the lobeglitazone-treated and vehicle-treated mice. ConclusionThese findings suggest that lobeglitazone has no detrimental effects on osteoblast biology and might not induce side effects in the skeletal system.
-
Citations
Citations to this article as recorded by  - Efficacy and safety of novel thiazolidinedione lobeglitazone for managing type-2 diabetes a meta-analysis
Deep Dutta, Saptarshi Bhattacharya, Manoj Kumar, Priyankar K. Datta, Ritin Mohindra, Meha Sharma
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2023; 17(1): 102697. CrossRef - Efficacy and safety of lobeglitazone, a new Thiazolidinedione, as compared to the standard of care in type 2 diabetes mellitus: A systematic review and meta-analysis
Shashank R. Joshi, Saibal Das, Suja Xaviar, Shambo Samrat Samajdar, Indranil Saha, Sougata Sarkar, Shatavisa Mukherjee, Santanu Kumar Tripathi, Jyotirmoy Pal, Nandini Chatterjee
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2023; 17(1): 102703. CrossRef - A Real-World Study of Long-Term Safety and Efficacy of Lobeglitazone in Korean Patients with Type 2 Diabetes Mellitus
Bo-Yeon Kim, Hyuk-Sang Kwon, Suk Kyeong Kim, Jung-Hyun Noh, Cheol-Young Park, Hyeong-Kyu Park, Kee-Ho Song, Jong Chul Won, Jae Myung Yu, Mi Young Lee, Jae Hyuk Lee, Soo Lim, Sung Wan Chun, In-Kyung Jeong, Choon Hee Chung, Seung Jin Han, Hee-Seok Kim, Ju-Y
Diabetes & Metabolism Journal.2022; 46(6): 855. CrossRef - Comparative Efficacy of Lobeglitazone Versus Pioglitazone on Albuminuria in Patients with Type 2 Diabetes Mellitus
Kyung-Soo Kim, Sangmo Hong, Hong-Yup Ahn, Cheol-Young Park
Diabetes Therapy.2021; 12(1): 171. CrossRef - Lobeglitazone: A Novel Thiazolidinedione for the Management of Type 2 Diabetes Mellitus
Jaehyun Bae, Taegyun Park, Hyeyoung Kim, Minyoung Lee, Bong-Soo Cha
Diabetes & Metabolism Journal.2021; 45(3): 326. CrossRef - Effect of lobeglitazone on motor function in rat model of Parkinson’s disease with diabetes co-morbidity
Kambiz Hassanzadeh, Arman Rahimmi, Mohammad Raman Moloudi, Rita Maccarone, Massimo Corbo, Esmael Izadpanah, Marco Feligioni
Brain Research Bulletin.2021; 173: 184. CrossRef - Comparison of the Effects of Various Antidiabetic Medication on Bone Mineral Density in Patients with Type 2 Diabetes Mellitus
Jeonghoon Ha, Yejee Lim, Mee Kyoung Kim, Hyuk-Sang Kwon, Ki-Ho Song, Seung Hyun Ko, Moo Il Kang, Sung Dae Moon, Ki-Hyun Baek
Endocrinology and Metabolism.2021; 36(4): 895. CrossRef - Xenogeneic native decellularized matrix carrying PPARγ activator RSG regulating macrophage polarization to promote ligament-to-bone regeneration
Xue Han, Lijun Liao, Tian Zhu, Yuchan Xu, Fei Bi, Li Xie, Hui Li, Fangjun Huo, Weidong Tian, Weihua Guo
Materials Science and Engineering: C.2020; 116: 111224. CrossRef - Diabetes pharmacotherapy and effects on the musculoskeletal system
Evangelia Kalaitzoglou, John L. Fowlkes, Iuliana Popescu, Kathryn M. Thrailkill
Diabetes/Metabolism Research and Reviews.2019;[Epub] CrossRef - The effects of diabetes therapy on bone: A clinical perspective
Karim G. Kheniser, Carmen M. Polanco Santos, Sangeeta R. Kashyap
Journal of Diabetes and its Complications.2018; 32(7): 713. CrossRef
- Clinical Study
- Characterization of Patients with Type 2 Diabetes according to Body Mass Index: Korea National Health and Nutrition Examination Survey from 2007 to 2011
-
Dong-Hwa Lee, Kyong Yeun Jung, Kyeong Seon Park, Kyoung Min Kim, Jae Hoon Moon, Soo Lim, Hak Chul Jang, Sung Hee Choi
-
Endocrinol Metab. 2015;30(4):514-521. Published online December 31, 2015
-
DOI: https://doi.org/10.3803/EnM.2015.30.4.514
-
-
3,606
View
-
42
Download
-
15
Web of Science
-
16
Crossref
-
 Abstract Abstract
 PDF PDF PubReader PubReader
- Background
The present study aimed to investigate the clinical characteristics of type 2 diabetes mellitus (T2DM) in Korean adults according to body mass index (BMI) and to analyze the association with cardiovascular disease (CVD). MethodsWe conducted a cross-sectional study of data from the Korea National Health and Nutrition Examination Survey from 2007 to 2011. A total of 3,370 patients with T2DM were divided into categories according to BMI. We conducted a comparison of the T2DM patient population composition by BMI category between different countries. We investigated the prevalence of awareness, treatment, and target control of T2DM according to BMI. ResultsPatients with T2DM had a higher BMI, and were more likely to have a history of CVD than healthy controls. For Korean adults with T2DM, 8% had BMI ≥30 kg/m2. By contrast, the population of patients with T2DM and BMI ≥30 kg/m2 was 72% in patients in the USA and 56% in the UK. The rate of recognition, treatment, and control has worsened in parallel with increasing BMI. Even in patients with BMI 25 to 29.9 kg/m2, the prevalence of CVD or high risk factors for CVD was significantly higher than in patients with BMI 18.5 to 22.9 kg/m2 (odds ratio, 2.07). ConclusionKorean patients with T2DM had lower BMI than those in Western countries. Higher BMI was associated with lower awareness, treatment, and control of diabetes, and a positive association was observed between CVD or high risk factors for CVD and BMI, even for patients who were overweight but not obese.
-
Citations
Citations to this article as recorded by  - Influenza vaccination trend and related factors among patients with diabetes in Korea: Analysis using a nationwide database
Dong-Hwa Lee, Bumhee Yang, Seonhye Gu, Eung-Gook Kim, Youlim Kim, Hyung Koo Kang, Yeong Hun Choe, Hyun Jeong Jeon, Seungyong Park, Hyun Lee
Frontiers in Endocrinology.2023;[Epub] CrossRef - Diet Quality Scores and Asthenoteratozoospermia Risk: Finding From a Hospital-Based Case–Control Study in China
Qi Cui, Hui-Han Wang, Qi-Jun Wu, Xiao-Bin Wang, Ren-Hao Guo, Xu Leng, Xiao-Ling Tan, Qiang Du, Bo-Chen Pan
Frontiers in Nutrition.2022;[Epub] CrossRef - Obesity definition for personalised treatment of type 2 diabetes Authors’ reply
Ildiko Lingvay, Priya Sumithran, Ricardo V Cohen, Carel W le Roux
The Lancet.2022; 399(10342): 2189. CrossRef - Secular trends and determinants of influenza vaccination uptake among patients with cardiovascular disease in Korea: Analysis using a nationwide database
Min Kim, Bumhee Yang, Seonhye Gu, Eung-Gook Kim, So Rae Kim, Kyeong Seok Oh, Woong-Su Yoon, Dae-Hwan Bae, Ju Hee Lee, Sang Min Kim, Woong Gil Choi, Jang-Whan Bae, Kyung-Kuk Hwang, Dong-Woon Kim, Myeong-Chan Cho, Hyun Lee, Dae-In Lee
Frontiers in Cardiovascular Medicine.2022;[Epub] CrossRef - Triglyceride glucose (TyG) index as a predictor of incident type 2 diabetes among nonobese adults: a 12-year longitudinal study of the Korean Genome and Epidemiology Study cohort
Byoungjin Park, Hye Sun Lee, Yong-Jae Lee
Translational Research.2021; 228: 42. CrossRef - Gamitaeeumjowee-Tang for weight loss in diabetic patients: A retrospective chart review
A-Reum Lee, Da-Yeon Lee, Min-Ji Kim, Hyang-Sook Lee, Ka-Hye Choi, Seo-Young Kim, Young-Woo Lim, Young-Bae Park
Journal of Korean Medicine.2021; 42(1): 46. CrossRef - Effect of cilostazol, a phosphodiesterase‐3 inhibitor, on coronary artery stenosis and plaque characteristics in patients with type 2 diabetes: ESCAPE study
Dong‐Hwa Lee, Eun Ju Chun, Tae Jung Oh, Kyoung Min Kim, Jae Hoon Moon, Sung Hee Choi, Kyong Soo Park, Hak Chul Jang, Soo Lim
Diabetes, Obesity and Metabolism.2019; 21(6): 1409. CrossRef - The Differential Role of Vitamin D in Type 2 Diabetes Management and Control in Minority Populations
Miyong To Kim, Kim Byeng Kim, Jisook Ko, Nicole Murry, David Levine, Ju-Young Lee
Journal of Immigrant and Minority Health.2019; 21(6): 1266. CrossRef - House dust mite and Cockroach specific Immunoglobulin E sensitization is associated with diabetes mellitus in the adult Korean population
Mee Kyoung Kim, Jee Sun Jeong, Kyungdo Han, Ki Hyun Baek, Ki-Ho Song, Hyuk-Sang Kwon
Scientific Reports.2018;[Epub] CrossRef - Long‐term effects on glycaemic control and β‐cell preservation of early intensive treatment in patients with newly diagnosed type 2 diabetes: A multicentre randomized trial
Suk Chon, Sang Youl Rhee, Kyu Jeung Ahn, Sei Hyun Baik, Yongsoo Park, Moon Suk Nam, Kwan Woo Lee, Soon Jib Yoo, Gwanpyo Koh, Dae Ho Lee, Young Seol Kim, Jeong‐Taek Woo
Diabetes, Obesity and Metabolism.2018; 20(5): 1121. CrossRef - Association between Body Weight Changes and Menstrual Irregularity: The Korea National Health and Nutrition Examination Survey 2010 to 2012
Kyung Min Ko, Kyungdo Han, Youn Jee Chung, Kun-Ho Yoon, Yong Gyu Park, Seung-Hwan Lee
Endocrinology and Metabolism.2017; 32(2): 248. CrossRef - Abnormal subchondral bone remodeling and its association with articular cartilage degradation in knees of type 2 diabetes patients
Yan Chen, Yong-Can Huang, Chun Hoi Yan, Kwong Yuen Chiu, Qingjun Wei, Jingmin Zhao, X Edward Guo, Frankie Leung, William W Lu
Bone Research.2017;[Epub] CrossRef - Social Networking Services-Based Communicative Care for Patients with Diabetes Mellitus in Korea
Hun-Sung Kim, Yoo Jeong, Sun Baik, So Yang, Tong Kim, Hyunah Kim, Hyunyong Lee, Seung-Hwan Lee, Jae Cho, In-Young Choi, Kun-Ho Yoon
Applied Clinical Informatics.2016; 07(03): 899. CrossRef - Pharmacological Management of Obesity in Patients with Type 2 Diabetes: An Update
Eun Ju Lee, Tae Nyun Kim
The Korean Journal of Obesity.2016; 25(3): 121. CrossRef - Response: Characterization of Patients with Type 2 Diabetes according to Body Mass Index: Korea National Health and Nutrition Examination Survey from 2007 to 2011 (Endocrinol Metab 2015;30:514-21, Dong-Hwa Lee et al.)
Sung Hee Choi
Endocrinology and Metabolism.2016; 31(2): 347. CrossRef - Letter: Characterization of Patients with Type 2 Diabetes according to Body Mass Index: Korea National Health and Nutrition Examination Survey from 2007 to 2011 (Endocrinol Metab 2015;30:514-21, Dong-Hwa Lee et al.)
Eun-Hee Cho
Endocrinology and Metabolism.2016; 31(2): 345. CrossRef
- Obesity and Metabolism
- Ectopic Fat Assessment Focusing on Cardiometabolic and Renal
Risk
-
Soo Lim
-
Endocrinol Metab. 2014;29(1):1-4. Published online March 14, 2014
-
DOI: https://doi.org/10.3803/EnM.2014.29.1.1
-
-
3,852
View
-
59
Download
-
36
Web of Science
-
36
Crossref
-
 Abstract Abstract
 PDF PDF PubReader PubReader
It is well known that people with high levels of body fat are at higher risk for
developing diabetes mellitus, kidney disease, and cardiovascular disorders.
Since individuals who are slightly overweight, or even individuals of normal
weight, can vary in body fat distribution, their metabolic profiles and the
degree of association of these profiles with cardiometabolic risk factors may
differ. Fat distribution might be more of a predictive factor for
cardiorenometabolic risk than obesity itself, which has led researchers to
investigate whether ectopic fat accumulation may partially account for the
development of cardiorenometabolic disorders. In addition to visceral obesity,
fat can accumulate in the liver and muscle, and these intrahepatic and
intramuscular lipid stores are associated with insulin resistance and adverse
metabolic phenotypes. More recently, pericardial fat, perivascular fat, and
perirenal fat were found to be associated with coronary atherosclerosis,
cardiovascular diseases, and kidney damage, respectively. Thus, regional fat
distribution may play a key role in understanding the development of
cardiorenometabolic diseases in nonobese people. -
Citations
Citations to this article as recorded by  - Renal stiffness measured by shear wave elastography and its relationship with perirenal fat in patients with chronic kidney disease
Yiming Li, Yongzhan Liu, Lili Gao, Chuan Tian
Journal of Clinical Ultrasound.2024; 52(1): 3. CrossRef - Characterization of Green and Yellow Papaya (Carica papaya) for Anti-Diabetic Activity in Liver and Myoblast Cells and Wound-Healing Activity in Fibroblast Cells
Haiwen Li, Obaid Ullah Beg, Ahmed Reza Rafie, Sadia Kanwal, Alexandra Ovalle-Cisneros, Milton Omar Faison, Rafat Ali Siddiqui
Nutrients.2023; 15(8): 1929. CrossRef - Association between fatty liver index and risk of end-stage renal disease stratified by kidney function in patients with type 2 diabetes: A nationwide population-based study
Goh Eun Chung, Kyungdo Han, Kyu-Na Lee, Jung Ho Bae, Sun Young Yang, Su-Yeon Choi, Jeong Yoon Yim, Nam Ju Heo
Diabetes & Metabolism.2023; 49(4): 101454. CrossRef - Perirenal Fat as a New Independent Prognostic Factor in Patients With Surgically Treated Clear Cell Renal Cell Carcinoma
Yiqing Du, Wenbo Yang, Huixin Liu, Caipeng Qin, Xu Tang, Tao Xu
Clinical Genitourinary Cancer.2022; 20(1): e75. CrossRef - The Influence of Obesity and Metabolic Health on Vascular Health
Eun-Jung Rhee
Endocrinology and Metabolism.2022; 37(1): 1. CrossRef - Obesity‐related glomerulopathy: Current approaches and future perspectives
José Ignacio Martínez‐Montoro, Enrique Morales, Isabel Cornejo‐Pareja, Francisco J. Tinahones, José Carlos Fernández‐García
Obesity Reviews.2022;[Epub] CrossRef - Neck circumference and waist circumference associated with cardiovascular events in type 2 diabetes (Beijing Community Diabetes Study 23)
Guang-Ran Yang, Ming-Xia Yuan, Gang Wan, Xue-Lian Zhang, Han-Jing Fu, Shen-Yuan Yuan, Liang-Xiang Zhu, Rong-Rong Xie, Jian-Dong Zhang, Yu-Ling Li, Yan-Hua Sun, Qin-Fang Dai, Da-Yong Gao, Xue-Li Cui, Jian-Qin Gao, Zi-Ming Wang, Ying-Jun Chen, Yong-Jin Li,
Scientific Reports.2021;[Epub] CrossRef - LKB1 Regulates Goat Intramuscular Adipogenesis Through Focal Adhesion Pathway
Yan Xiong, Yuxue Wang, Qing Xu, An Li, Yongqi Yue, Yan Ma, Yaqiu Lin
Frontiers in Physiology.2021;[Epub] CrossRef - Serum Uric Acid and Diabetes: From Pathophysiology to Cardiovascular Disease
Niki Katsiki, George D. Dimitriadis, Dimitri P. Mikhailidis
Current Pharmaceutical Design.2021; 27(16): 1941. CrossRef - Is Epidural Fat Affected by Peripheric or Visceral Adipose Tissue? A Radiologic View
Nilüfer AYLANÇ, Mustafa REŞORLU, Gürhan ADAM
Konuralp Tıp Dergisi.2019; 11(1): 41. CrossRef - Perirenal Adiposity and Other Excessive Intra- and Peri-Organ Fat Depots: What Is the Connection?
Niki Katsiki, George Dimitriadis, Dimitri P. Mikhailidis
Angiology.2019; 70(7): 581. CrossRef - Letter: Association of Z-Score of the Log-Transformed A Body Shape Index with Cardiovascular Disease in People Who Are Obese but Metabolically Healthy: The Korea National Health and Nutrition Examination Survey 2007-2010 (J Obes Metab Syndr 2018;27:158-65
Eun-Jung Rhee
Journal of Obesity & Metabolic Syndrome.2019; 28(2): 139. CrossRef - Determinants of Bone Mass and Insulin Resistance in Korean Postmenopausal Women: Muscle Area, Strength, or Composition?
Hye-Sun Park, Jung Soo Lim, Sung-Kil Lim
Yonsei Medical Journal.2019; 60(8): 742. CrossRef - FIB-4 Index and Diabetes Mellitus Are Associated with Chronic Kidney Disease in Japanese Patients with Non-Alcoholic Fatty Liver Disease
Yuya Seko, Kohta Yano, Aya Takahashi, Shinya Okishio, Seita Kataoka, Keiichiroh Okuda, Naoki Mizuno, Masashi Takemura, Hiroyoshi Taketani, Atsushi Umemura, Taichiro Nishikawa, Kanji Yamaguchi, Michihisa Moriguchi, Takeshi Okanoue, Yoshito Itoh
International Journal of Molecular Sciences.2019; 21(1): 171. CrossRef - Being Metabolically Healthy, the Most Responsible Factor for Vascular Health
Eun-Jung Rhee
Diabetes & Metabolism Journal.2018; 42(1): 19. CrossRef - The persistence of fatty liver has a differential impact on the development of diabetes: The Kangbuk Samsung Health Study
Ji Cheol Bae, Ji Min Han, Jung Hwan Cho, Hyemi Kwon, Se Eun Park, Cheol-Young Park, Won-Young Lee, Ki-Won Oh, Sam Kwon, Sung-Woo Park, Eun Jung Rhee
Diabetes Research and Clinical Practice.2018; 135: 1. CrossRef - Changes of renal sinus fat and renal parenchymal fat during an 18-month randomized weight loss trial
Hila Zelicha, Dan Schwarzfuchs, Ilan Shelef, Yftach Gepner, Gal Tsaban, Lilac Tene, Anat Yaskolka Meir, Avital Bilitzky, Oded Komy, Noa Cohen, Nitzan Bril, Michal Rein, Dana Serfaty, Shira Kenigsbuch, Yoash Chassidim, Benjamin Sarusi, Joachim Thiery, Uta
Clinical Nutrition.2018; 37(4): 1145. CrossRef - Association between abdominal obesity and increased risk for the development of hypertension regardless of physical activity: A nationwide population‐based study
Eun‐Jung Rhee, Jung‐Hwan Cho, Hyemi Kwon, Se‐Eun Park, Jin‐Hyung Jung, Kyung‐Do Han, Yong‐Gyu Park, Hye Soon Park, Yang‐Hyun Kim, Soon‐Jib Yoo, Won‐Young Lee
The Journal of Clinical Hypertension.2018; 20(10): 1417. CrossRef - Mesenchymal stem cells in obesity: insights for translational applications
Kenichi Matsushita, Victor J Dzau
Laboratory Investigation.2017; 97(10): 1158. CrossRef - Additive effect of non-alcoholic fatty liver disease on the development of diabetes in individuals with metabolic syndrome
Ji Cheol Bae, Soo Kyoung Kim, Ji Min Han, Sam Kwon, Da Young Lee, Jihyun Kim, Se Eun Park, Cheol-Young Park, Won-Young Lee, Ki-Won Oh, Sung-Woo Park, Eun Jung Rhee
Diabetes Research and Clinical Practice.2017; 129: 136. CrossRef - Development of chronic kidney disease in patients with non-alcoholic fatty liver disease: A cohort study
Dong Hyun Sinn, Danbee Kang, Hye Ryoun Jang, Seonhye Gu, Soo Jin Cho, Seung Woon Paik, Seungho Ryu, Yoosoo Chang, Mariana Lazo, Eliseo Guallar, Juhee Cho, Geum-Youn Gwak
Journal of Hepatology.2017; 67(6): 1274. CrossRef - Mesenchymal Stem Cells and Metabolic Syndrome: Current Understanding and Potential Clinical Implications
Kenichi Matsushita
Stem Cells International.2016; 2016: 1. CrossRef - LDL-C/apoB and HDL-C/apoA-1 ratios predict incident chronic kidney disease in a large apparently healthy cohort
Ji Cheol Bae, Ji Min Han, Sam Kwon, Jae Hwan Jee, Tae Yang Yu, Moon Kyu Lee, Jae Hyeon Kim
Atherosclerosis.2016; 251: 170. CrossRef - Sirtuin 3 (SIRT3) Regulates α-Smooth Muscle Actin (α-SMA) Production through the Succinate Dehydrogenase-G Protein-coupled Receptor 91 (GPR91) Pathway in Hepatic Stellate Cells
Ying Hui Li, Dae Hee Choi, Eun Hye Lee, Su Ryeon Seo, Seungkoo Lee, Eun-Hee Cho
Journal of Biological Chemistry.2016; 291(19): 10277. CrossRef - Deletion of angiotensin II type 2 receptor accelerates adipogenesis in murine mesenchymal stem cells via Wnt10b/beta-catenin signaling
Kenichi Matsushita, Yaojiong Wu, Richard E Pratt, Victor J Dzau
Laboratory Investigation.2016; 96(8): 909. CrossRef - Increased risk of subclinical atherosclerosis associated with high visceral adiposity index in apparently healthy Korean adults: the Kangbuk Samsung Health Study
Hye-Jeong Park, Jihyun Kim, Se Eun Park, Cheol-Young Park, Won-Young Lee, Ki-Won Oh, Sung-Woo Park, Eun-Jung Rhee
Annals of Medicine.2016; 48(6): 410. CrossRef - The Roles of Adipokines, Proinflammatory Cytokines, and Adipose Tissue Macrophages in Obesity-Associated Insulin Resistance in Modest Obesity and Early Metabolic Dysfunction
Yea Eun Kang, Ji Min Kim, Kyong Hye Joung, Ju Hee Lee, Bo Ram You, Min Jeong Choi, Min Jeong Ryu, Young Bok Ko, Min A. Lee, Junguee Lee, Bon Jeong Ku, Minho Shong, Ki Hwan Lee, Hyun Jin Kim, Guillermo López Lluch
PLOS ONE.2016; 11(4): e0154003. CrossRef - Neck circumference and future cardiovascular events in a high-risk population—A prospective cohort study
Yingnan Dai, Xiaojing Wan, Xin Li, Enze Jin, Xueqi Li
Lipids in Health and Disease.2016;[Epub] CrossRef - Anti-obesity Effects of Ethanolic Extract of Polygonatum sibiricum Rhizome in High-fat Diet-fed Mice
Jong-Hee Ko, Woo-Jin Jeon, Hyuk-Sang Kwon, Seung-Woo Yeon, Jae-Hoon Kang
Korean Journal of Food Science and Technology.2015; 47(4): 499. CrossRef - Articles in 'Endocrinology and Metabolism' in 2014
Won-Young Lee
Endocrinology and Metabolism.2015; 30(1): 47. CrossRef - Anti-diabetic efficacy of KICG1338, a novel glycogen synthase kinase-3β inhibitor, and its molecular characterization in animal models of type 2 diabetes and insulin resistance
Kyoung Min Kim, Kuy-Sook Lee, Gha Young Lee, Hyunjin Jin, Eunice Sung Durrance, Ho Seon Park, Sung Hee Choi, Kyong Soo Park, Young-Bum Kim, Hak Chul Jang, Soo Lim
Molecular and Cellular Endocrinology.2015; 409: 1. CrossRef - Effects ofPolygonatum sibiricumrhizome ethanol extract in high-fat diet-fed mice
Jong-Hee Ko, Hyuk-Sang Kwon, Jong-Min Yoon, Jong-Su Yoo, Hyeon-Soo Jang, Ji-Young Kim, Seung-Woo Yeon, Jae-Hoon Kang
Pharmaceutical Biology.2015; 53(4): 563. CrossRef - Lactisole inhibits the glucose-sensing receptor T1R3 expressed in mouse pancreatic β-cells
Kunihisa Hamano, Yuko Nakagawa, Yoshiaki Ohtsu, Longfei Li, Johan Medina, Yuji Tanaka, Katsuyoshi Masuda, Mitsuhisa Komatsu, Itaru Kojima
Journal of Endocrinology.2015; 226(1): 57. CrossRef - Improvement of Nonalcoholic Fatty Liver Disease With Carnitine-Orotate Complex in Type 2 Diabetes (CORONA): A Randomized Controlled Trial
Ji Cheol Bae, Won Young Lee, Kun Ho Yoon, Joong Yeol Park, Hyun Sik Son, Kyung Ah Han, Kwan Woo Lee, Jeong Taek Woo, Young Cheol Ju, Won Jae Lee, Yoon Young Cho, Moon-Kyu Lee
Diabetes Care.2015; 38(7): 1245. CrossRef - Letter: The Risk Factors of Sarcopenia among Korean Elderly Men: Based on 2009 Korean National Health and Nutrition Examination Survey Data (Korean J Obes 2014;23:23-31)
Ho Cheol Hong
The Korean Journal of Obesity.2014; 23(2): 136. CrossRef - The association between ectopic fat in the pancreas and subclinical atherosclerosis in type 2 diabetes
Mee Kyoung Kim, Hyun Ji Chun, Jin Hee Park, Dong Myung Yeo, Ki-Hyun Baek, Ki-Ho Song, Dong Jin Chung, Hyuk-Sang Kwon
Diabetes Research and Clinical Practice.2014; 106(3): 590. CrossRef
- Metabolic Syndrom and Perosixome Proliferator-activated Receptor gamma.
-
Soo Lim, Kyong Soo Park
-
J Korean Endocr Soc. 2004;19(3):256-266. Published online June 1, 2004
-
-
-
 Abstract Abstract
 PDF PDF
- No abstract available.
- Determinants of Limb-Bone Mineral Density in Healthy Men and Women Aged over 50 in Rural Area.
-
Soo Lim, Chan Soo Shin, Ki Sook Kim, Soo Youn Kim, Eun Joo Bang, Eun Kyung Shin, Hye Ran Choi, Moon Ho Chung, Sung Il Cho
-
J Korean Endocr Soc. 2003;18(2):193-205. Published online April 1, 2003
-
-
-
 Abstract Abstract
 PDF PDF
- BACKGROUND
Many studies have shown a strong inverse relationship between the bone mineral density (BMD) and osteoporotic fractures, with a doubling in the incidence of fractures for each standard deviation reduction in the BMD. Newer peripheral densitometry devices have recently been developed, with the advantages of a low cost and increased portability. In addition, studies focusing on the osteoporosis of rural populations are rare. The authors assessed the factors related with the BMD in rural areas, using peripheral bone densitometry. METHODS: 23 men (68.4+/-9.2[mean age+/-SD] years) and 32 women (63.9+/-8.3 years), living in rural areas, voluntarily participated in this community-based study. The BMD of the distal radius (BMDr) and calcaneus (BMDc) were measured using peripheral dual-energy X-ray absorptiometry. The BMI, waist to hip ratio, body composition, blood pressure, lipids, fasting glucose and insulin were measured. The sociodemographic characteristics and physical activities were investigated using questionnaires. RESULTS: 21.7% of the men and 34.4% of the women were diagnosed with osteoporosis according to the WHO definition. The BMDr and BMDc were 0.46+/-0.08 and 0.46+/-0.11 and 0.34+/-0.07 and 0.33+/-0.08g/cm2 in the men and women, respectively. In the men, age, BMI, physical activity and smoking were correlated with the BMDr, and age, lean body mass, physical activity, TV watching and smoking with the BMDc. In the women, age, weight and lean body mass were correlated with the BMDr, and age, weight, BMI, waist circumference, fat mass, lean body mass and year since menopause with the BMDc. From a multiple regression analysis, age and smoking in men, and year since menopause and lean body mass in women, respectively, had independent effects on the BMD. CONCLUSION: In the rural community studied, osteoporosis was as highly prevalent as in urban communities. Of the determinants for the BMD, smoking for men, and lean body mass for women, were modifiable factors. Education for quitting smoking in men, and maintenance of optimal weight in women, are required to prevent osteoporosis in rural areas.
- Metabolic Syndrome.
-
Min Kyong Moon, Young Min Cho, Soo Lim, Kyong Soo Park, Hong Kyu Lee
-
J Korean Endocr Soc. 2003;18(2):105-119. Published online April 1, 2003
-
-
-
 Abstract Abstract
 PDF PDF
- No abstract available.
- The Correlation of Plasma Homocysteine and Mitochondrial DNA Content in Peripheral Blood in Healthy Women.
-
Soo Lim, Won Shik Shin, Kyong Soo Park, Seong Yeon Kim, Jong Ho Lee, Mi Ja Yim, Ji Hyun Song, Hong Kyu Lee
-
J Korean Endocr Soc. 2000;15(2):248-261. Published online January 1, 2001
-
-
-
 Abstract Abstract
 PDF PDF
- BACKGROUND
Hyperhomocysteinemia is an independent risk factor for cardiovascular diseases. Previous reports showed that homocysteine damages mitochondrial gene expression, function and structure. In recent years, homocysteine and mitochondrial DNA (mtDNA) content are reported to relate with insulin resistance. The aim of this study is to investigate the correlation of plasma homocysteine level and mitochondrial DNA content in peripheral blood. METHODS: The mtDNA content, homocysteine and insulin resistance parameters were measured in healthy women (n=60). Plasma homocysteine level was measured by ion-exchange chromatography method and the mtDNA content in peripheral blood was measured by real time PCR method using ABI Prism 7700 machine. RESULTS: Significant correlation was found between homocysteine and mtDNA content (r=-0.507, p<0.05). Homocysteine was correlated with age (r=0.397), cholesterol (r=0.327), LDL-cholesterol (r=0.318), apolipoprotein B (r=0.387), HbA1c (r=0.274) positively and folate (r=-0.262), apolipoprotein A1 (r=-0.293), VO2max (r=-0.332) negatively. Mitochondrial DNA content was correlated with age (r=-0.535), BMI (r=-0.397), cholesterol (r=-0.340), LDL-cholesterol (r=-0.319), apolipoprotein B (r=-0.367) negatively and apolipoprotein A1 (r=0.346), lactate (r=0.307), VO2max (r=0.308) positively. All correlations were statistically significant(p<0.05). CONCLUSION: In this study, plasma homocysteine level was related with mitochondrial DNA content negatively and these two factors are estimated to be concerned with insulin resistance.
|